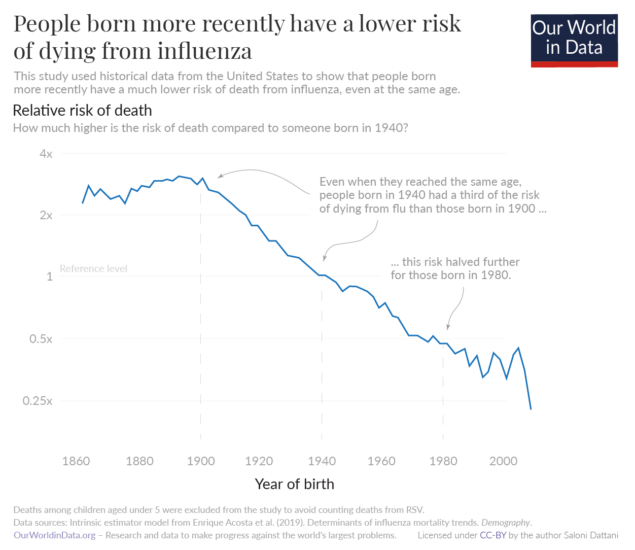
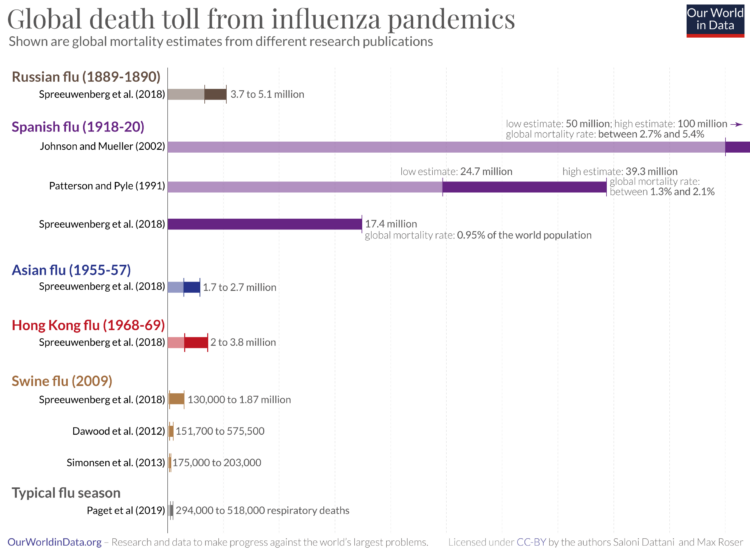
Seasonal flu is a contagious illness caused by the influenza virus. It kills around 400,000 people from respiratory disease on average each year. In large pandemics, when new strains have evolved, the death toll has been much higher.
Yet, data on the flu is limited. With better testing, countries could improve their response to flu epidemics. It could help to rapidly identify new strains, detect epidemics early, and design better-matched vaccines to target flu strains circulating in the population.
This page therefore shows estimates of deaths during seasonal flu epidemics, historical flu pandemics, patterns of flu seasons in different countries, and confirmed cases of flu and flu-like symptoms across the world.
It also includes our Flu Explorer, a resource for epidemiologists, infectious disease researchers, and public health experts to monitor the global spread of the influenza virus.
Key insights on Influenza
Explore our data on influenza
Why we provide this Influenza Data Explorer
With this Flu Explorer, we aim to provide a helpful resource for epidemiologists, infectious disease researchers, and public health experts to understand the global spread of the influenza virus.
It differs from our widely-used infectious diseases projects, such as the COVID-19 Explorer and the Mpox Explorer. These tools are designed for a broad audience. Unfortunately, flu data is incomplete in many ways, making it harder to communicate. This tool is therefore designed for users with pre-existing knowledge to navigate effectively the complex data published by the World Health Organization.
The explorer also highlights the significant gaps in influenza data. It is an important reminder of the need to improve data collection and reporting.